Bioprint-Boosting Human Reproduction
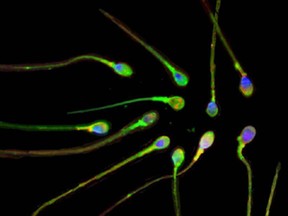
"A human testicular biopsy from a single donor with NOA [non-obstructive azoospermia] was dissociated into single cells [and then] expanded in vitro and 3-D bioprinted into tubular structures that resemble the tiny tubes that produce sperm.""[The research] may carry future potential for disease modelling and regenerative opportunities in a personalized medicine framework."Dr. Ryan Flannigan, urology assistant professor, University of British Columbia/Weill Cornell Medicine associate
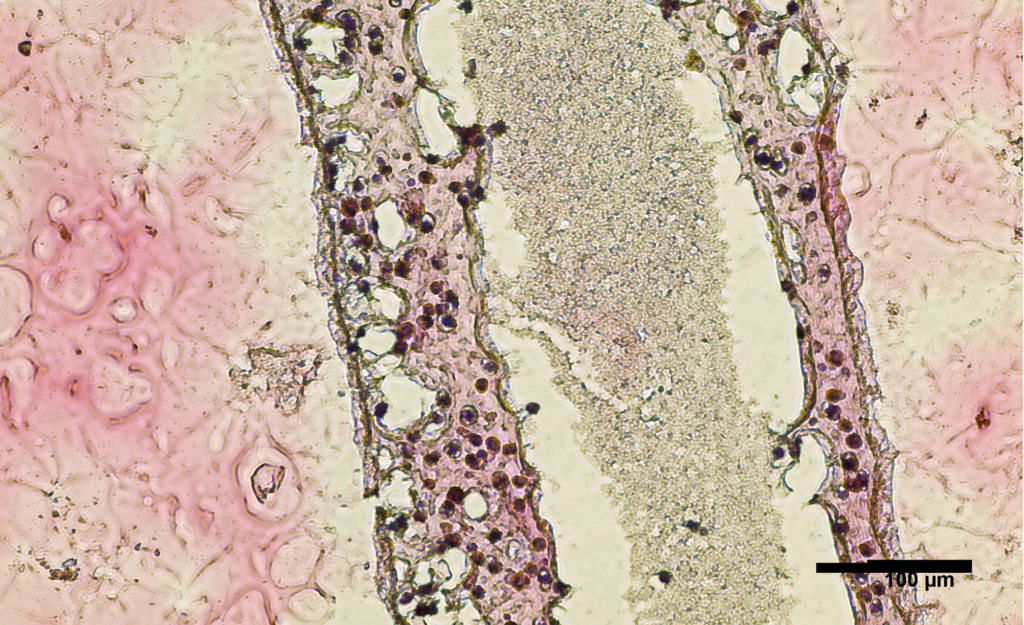 |
| Cross section of human testicular cells 3D printed into a tubular structure. |
Infertility is a problem faced by one in six couples in Canada, with 30 percent of such cases reflecting an inability to conceive attributable to the male partner. According to the Public Health Agency of Canada there are many causes of male infertility, among them poor sperm quality, low sperm count, or lack of sperm, a history of sexually transmitted infection like Chlamydia or hormonal imbalances.
That is not an exhaustive list to explain male infertility; other causes both for men and women can be traced to tobacco and alcohol use, being underweight or overweight, and cancer treatments such as chemotherapy, radiation and/or surgery. Included as well can be chronic conditions such as diabetes, including their medical treatments.
Nature is complex and she approves of ideal conditions for reproduction though she is not herself immune to producing occasional imperfect specimens.
While some forms of male infertility are correctable through appropriate treatment, even men with untreatable forms of infertility may now be on the brink of seeing research succeeding to convert into a potential treatment that overcomes all those other obstacles, thanks to researchers at the University of British Columbia.
 |
With his team of researchers, Dr.Flannigan decided to study the feasibility and potential of 3-D bioprinting of spermatogenic modelling. In the process discovering sperm production was indeed possible, given the success of their early trials. The team retrieved stem cells from a 31-year-old NOA patient to culture new cells which in turn showed a 93.4 percent viability in 24 hours.
These results were 3D printed into a petri dish. Non-obstructive azoospermia (NOA) a condition where no sperm is to be found in the ejaculate, has responded to reversal through surgery in some men, yet there is only a 50 percent success rate with the conventional surgical procedure.
Titled Using Clinically Derived Human Tissue to 3D Bioprint Personalized Testicular Tubules For in-Vitro Culturing, the research report noted following 12 days of observation saw the cells survive. Well enough so that the researchers now 'coach' the cells to produce sperm. Should that process succeed, the sperm should function for use in inseminating a viable egg.
 |
| Dr. Ryan Flannigan and research assistant Meghan Robinson with bioprinter |
Labels: Human Reproduction, Research, Spermatozoa Bioprinting

0 Comments:
Post a Comment
<< Home