DCD (Donation after Circulatory Death) Heart Transplants
"The thing that people need to get their heads around is that, in order to do DCD hearts -- heart transplants after the heart has stopped beating -- the heart has to start beating again.""It can either beat again outside the body, in this perfusion system or it can beat again inside the body."
"And the question is, because it's a more complicated procedure, because there are biological realities and there are ethical issues, the question will be for Canada going forward -- and I don't have the answer for you now -- can we do normothermic regional perfusion in Canada for DCD hearts? And if so, how to do it consistent with existing pratices and the medical, ethical and legal safeguards that should be in place."
"But, I think conceptually, in the world, we're evolving toward a brain-based concept of death. Would it fulfill our criteria for death? I can't answer that yet. There's both research and policy work that needs to be done to answer that question."
Dr. Sam Shemie, critical care doctor, medical adviser, Canadian Blood Services
 |
"We need to be certain that there is no brain perfusion following the resumption of circulation in the donor body. We also need to be certain that we have accepted that resuming circulation in the body does not invalidate the determination of death. And the critical-care community, in the large part, would accept that, I think. But more work is to be done before this can occur in Ontario."
"In culture, in a variety of symbolic ways, the heart means something special. Up until now, we've not been able to recover and transplant the heart in this donation, and many families have expressed disappointment in that."
"We are dealing with a group of people who consent to organ donation that are tremendously courageous and generous. They want to give the most that they can give."
Dr. Robert Truog, bioethicist pediatrician, U.S.
"So, it's probably a storm in a teacup [fears that] folks might wake up, or some such thing."
"And what we've seen is that we can restore that blood supply within four minutes of the patient arriving in the operating room after declaration of death."
Dr. Stephen Large, surgeon, Papworth Hospital, Cambridge, England
 |
Up to the present time, the delicate issue of donor hearts for transplant have been obtained from people whom medical science has declared brain-stem dead, a condition under which they are considered to be both medically and legally dead, even as their hearts remain capable of beating. The problem arises with the shortage of transplant-capable hearts from brain-dead donors. And a new technique has arisen which has become feasible for increasing the number of hearts for transplant at a crucial time of shortage.
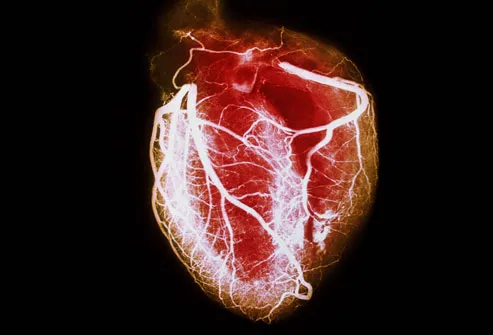
A portable device called a "heart-in-a-box" which is a perfusion machine somewhat similar in appearance to a mini-ICU where blood collected from the donor is pumped through an oxygenator and into the heart, has presented as part of another option. It is a technique whereby hearts from organ donors whose hearts have stopped beating, are restarted before transplantaton. Beating and "breathing", the disembodied heart can be viable inside the sterile box for up to 12 hours.
The method is in use in Australia and the U.K. In Britain doctors proceed once life support is withdrawn from a donor following that brief window when the heart no longer beats and doctors, having waited the obligatory five minutes before death is declared -- when no pulse, no heartbeat is detected, nor chance the heart may spontaneously begin beating again -- the body is removed to the operating chamber where surgeons cut into the sternum, clamp the main arteries and connect the body to a machine designed to take over the work of the heart and lungs.
This machine with its specialized engineering has been named ECMO, extracorporeal membrane oxygenation. This stage completed, an incision is made through the abdomen wall, blood is re-circulated to the thorax and abdomen, and the heart is "revived"; the person is dead, but the heart is once again beating. In twenty minutes' time the heart is taken from the machine pumping on its own while within the corpse. The heart is injected with a cooling solution, extracted, and placed within the perfusion device for transport to the hospital where the transplant patient is awaiting a new heart.
The Canadian Blood Services and Trillium Gift of Life Network in Ontario conferred to develop expert guidance in determining conditions where "donations" prepared in such a manner could be done in Canada. Where, once life support is withdrawn, the heart no longer beats, organ procurement commences. DCD donors account for 25 percent of all donations in Canada, resulting in a gratifying increase in donor kidneys, livers and lungs. Now, Canada awaits the addition of hearts to the new process, since one so successful with other organs fails with hearts.
The new process solves the problem of the heart contracting once life support is withdrawn, and starving of oxygen and blood. As the muscle cells begin to die, blood pressure drops leaving the heart to go into cardiac arrest; its response to a period without blood flow and oxygen. A conundrum has developed with respect to the new system called normothermic regional perfusion in that if death is defined as irreversible cessation of circulatory and respiratory function, once circulation is restored, how can the person be considered dead?
In response to which Dr. Truog notes that simply because a heart cannot restart on its own does not denote it cannot be restarted; that people are creating an imagined problem over the determination of permanence. Circulation to the brain, he argues along with other experts, is what most matters. If you "reanimate" the heart, the query remains, is there a remote opportunity for the brain to be reanimated, even if major vessels are clamped, cut and tied off?
The very question of reanimating dead hearts elicits a squeamish response from many. Some argue that restarting the heart has implications of death never having occurred, or that retrieval of the heart would amount to a violation of the "Dead Donor Rule", holding that organs must not be procured until the individual is dead. Two Harvard doctors argue in the journal Circulation: Heart Failure, that the act of reviving the heart will not alter its biological condition at the moment that death was declared; that it would not "toggle the state of the donor between dead and alive".
Since major blood vessels feeding the brain have been clamped, "the donor can be considered brain-dead before the donor heart is reanimated", they concluded. About 25 percent of adults in Canada die as they wait on, or are removed from the waiting list, once they become too ill for transplant. Leaving about 150 adult heart transplants concluded annually in Canada. "So even if you increase it by ten or twenty percent, that's significant", stated Dr. Shemie.
"Heart transplantation remains the preferred option for improving quality of life and survival for patients suffering from end-stage heart failure. Unfortunately, insufficient supply of cardiac grafts has become an obstacle. Increasing organ availability with donation after circulatory death (DCD) may be a promising option to overcome the organ shortage. Unlike conventional donation after brain death, DCD organs undergo a period of warm, global ischemia between circulatory arrest and graft procurement, which raises concerns for graft quality." "Nonetheless, the potential of DCD heart transplantation is being reconsidered, after reports of more than 70 cases in Australia and the United Kingdom over the past 3 years. Ensuring optimal patient outcomes and generalized adoption of DCD in heart transplantation, however, requires further development of clinical protocols, which in turn require a better understanding of cardiac ischemia-reperfusion injury and the various possibilities to limit its adverse effects. Thus, we aim to provide an overview of the knowledge obtained with preclinical studies in animal models of DCD heart transplantation, to facilitate and promote the most effective and efficient advancement in preclinical research. A literature search of the PubMed database was performed to identify all relevant preclinical studies in DCD heart transplantation. Specific aspects relevant for DCD heart transplantation were analyzed, including animal models, graft procurement and storage conditions, cardioprotective approaches, and graft evaluation strategies. Several potential therapeutic strategies for optimizing graft quality are identified, and recommendations for further preclinical research are provided."
Circulation: Heart Failure
Labels: DCD Heart Transplants, Health, Medicine, Organ Transplants

0 Comments:
Post a Comment
<< Home