Advances in Post-Heart Attack Heart Muscle Repair
"This injectable material is the first in the world prepared using human collagen."
"As a standalone therapy, we believe the rHCI gel performs better than any cell-based therapies or pharmacological treatment currently available, allowing for easier future translation to the clinic."
"The treatment works, in part, by increasing the number of cardiac muscle cells and blood capillaries in the tissue surrounding the damaged area. The gel also promotes the recruitment of more wound healing cells to the site of injury."
"We had to complete it [research study] many times because we couldn't believe it [the findings]."
"[The heart institute's BioEngineering and Therapeutic Solutions team [BEaTS] are hopeful their human collagen gel will one day lead to a recovery of heart function and prevent heart failure in humans, but more testing is required."
Dr.Emilio Alarcon, Scientist, Division of Cardiac Surgery, Director, Bio-nanomaterials Chemistry and Engineering Laboratory, University of Ottawa Heart Institute
"As people with damaged hearts are living longer, the incidence of heart failure is increasing. Therefore, a treatment capable of recovering cardiac function and preventing heart failure would have a tremendous health and societal impact worldwide."
"The therapy developed here in Ottawa by the BEaTS team is a promising approach to accomplishing this."
Dr. Marc Ruel, Division Head of Cardiac Surgery at the UOHI
 |
| Gordon Keller Lab. Heart cells beating in a culture dish |
Added to which people living away from urban areas, remote from health care, along with individuals who fail to seek out immediate treatment or have no idea they've suffered a heart attack, are likelier than others to suffer heart muscle damage.
Within Canada an estimated 600,000 patients cope with managing advanced heart failure, with health-care costs amounting to over $2.8 billion annually. This is a situation compounded by the fact that with professional health care of the greatest quality available, people are living longer and inevitably the numbers of people being treated with advanced heart failure through therapeutic means will rise even while treatment cost will inevitably increase.
Any new protocols that aid in prolonging life and making the condition more manageable would be a huge assist in terms of quality of life for patients and in alleviating the burden somewhat on the health care system.
Dr. Alarcon and his colleagues at the Heart Institute have been absorbed for years in the concept of a remedial gel for heart patients post-heart attack. They had developed a gel containing human collagen able to repair damaged hearts in laboratory mice. Because of the startlingly positive results, they methodically and studiously repeated the study, to find that randomized, blinded results validated their aspirational success.
The five years spent dedicated to the project saw publication in the journal Nature Communications, with Dr. Alarcon and Dr. Erik Suuronen, a scientist in the Division of Cardiac Surgery, and director of its Biomaterials and Regeneration program, as lead authors. The injectable gel their research produced is now viewed as an unprecedented leap toward addressing cardiac muscle repair following a heart attack, with the use of the injectable material recognized as the first ever prepared with the use of human collagen.
The gel is designed for injection directly into patients' hearts to help heal damaged heart tissue following a heart attack. The research team feels the gel is a vast improvement over any other cell-based therapies or drug treatments reflecting current therapeutic protocols. The gel treatment, explained Dr. Alarcon, works through increasing the number of cardiac muscle cells and blood capillaries in the tissue surrounding damaged areas of the heart as the gel helps to produce greater numbers of wound-healing cells to promote repair.
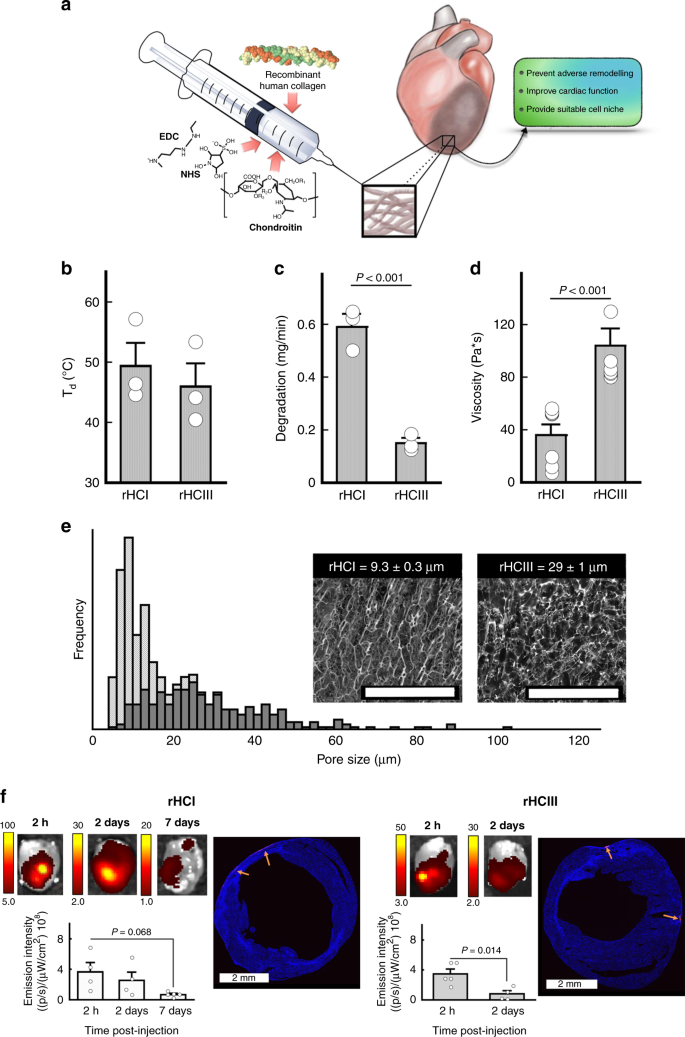
Abstract: Despite the success of current therapies for acute myocardial infarction (MI), many patients still develop adverse cardiac remodeling and heart failure. With the growing prevalence of heart failure, a new therapy is needed that can prevent remodeling and support tissue repair. Herein, we report on injectable recombinant human collagen type I (rHCI) and type III (rHCIII) matrices for treating MI. Injecting rHCI or rHCIII matrices in mice during the late proliferative phase post-MI restores the myocardium’s mechanical properties and reduces scar size, but only the rHCI matrix maintains remote wall thickness and prevents heart enlargement. rHCI treatment increases cardiomyocyte and capillary numbers in the border zone and the presence of pro-wound healing macrophages in the ischemic area, while reducing the overall recruitment of bone marrow monocytes. Our findings show functional recovery post-MI using rHCI by promoting a healing environment, cardiomyocyte survival, and less pathological remodeling of the myocardium.
 |
Injectable human recombinant collagen matrices limit adverse remodeling and improve cardiac function after myocardial infarction Nature Communications |
Labels: Health, Heart Disease, Research, Therapeutic Treatments

0 Comments:
Post a Comment
<< Home