The COVID-Induced Black Fungus Epidemic in India
"This new variant is causing damage to the beta cells in the pancreas, which produce insulin and regulate blood glucose levels."We need more investigation into this --- around 40 percent more patients are developing diabetes after having COVID-19 during this second wave [of COVID to hit India]."Dr.Shailesh Kothalkar, Ear, nose and throat surgeon (ENT), Seven Star Hospital, Maharashtra state, India"I have seen 45 [mucormycosis] patients in my entire career and now we have had 66 patients admitted in just one month.""Over the last five days, we've barely slept, we've done 40 surgeries."Shrinivas Chavan, head, ENT department, Grant Medical College and Sir JJ Hospital, Mumbai
 | |
| Mucormycosis is rapidly fatal without prompt diagnosis.’ A nurse treats a patient suffering from mucormycosis in Jaipur, India. Photograph: Rebecca Conway/Getty Images |
COVID has any number of surprises backgrounding the prodigious efforts on the part of the medical community, research scientists and government health departments to gain control over the virus as it swiftly mutates, progressing to new, more infectious and serious strains to confound and befuddle efforts to come to grips with its vicious presence, spreading from one geographic location to another, introducing new variants to form the basis of new, more dangerous outbreaks.
Hundreds of people have now died from the gruesome effects of the flesh-eating black fungus disease rampant across India, which appears to have hitched a ride on the Indian variant now known as Delta. Which has been the cause of unprecedented damage to the pancreas of otherwise-healthy people, in turn triggering sudden-onset diabetes resulting in soaring blood glucose levels on which the fungus thrives. Mucormycosis cases has seen the fungal infection causing nose blackening or discolouration, blurred or double vision, chest pain, difficulties breathing and coughing up blood.
Public Health England issued a report finding the dominant Delta strain to be likelier to lead to increased hospital treatment requirements than the Alpha variant first detected in the southeastern county of Kent. In ten hospitals sprawled across the western Indian state of Maharashtra, doctors are treating patients among the 11,000 people now known to have been struck down by the aggressive infection post-COVID-recovery.
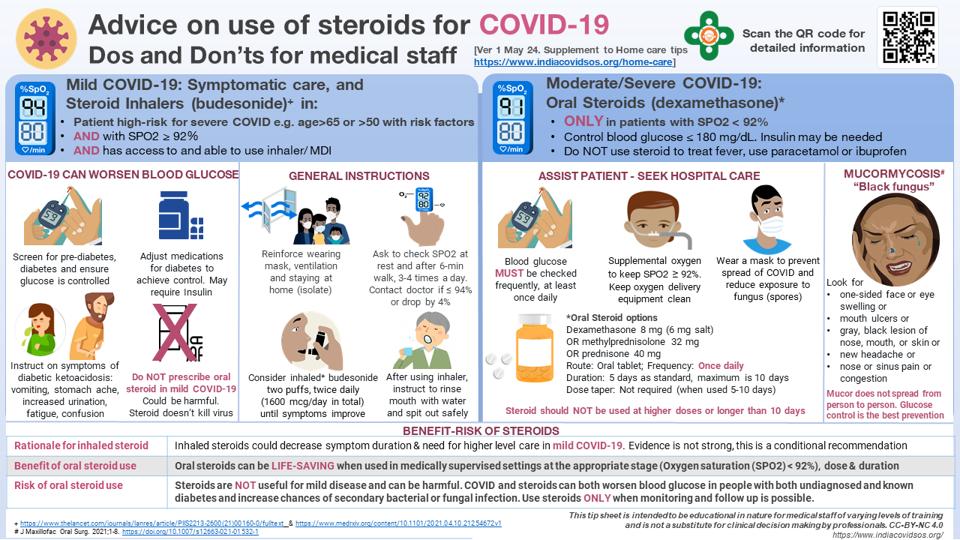
Initially doctors believed over-prescription of steroids for COVID treatment, an inexpensive, effective treatment to counter severe cases which can also suppress the immune system, was responsible for the sudden explosion in black fungus cases. Exhausted doctors across Maharashtra state warn that while long-term exposure to steroids was a contributory factor for some patients, mucormycosis cases exploded among diabetes patients only once the Delta variant emerged.
Before March 1, 41 cases of black fungus were recorded worldwide. There has been a spate of cases of coronavirus-induced mucormycosis recorded in India's neighbours, Nepal and Bangladesh among them, where Delta has become dominant. Mucormycosis is caused by a mucor found commonly in soils and decaying vegetation leading to the fungus that infects the sinuses and lungs of an immuno-compromised individual before spreading to the brain.
According to the doctors working on the situation, early detection reliant on regular blood glucose screening among recovered COVID-19 patients is seen as critical in a bid to control the fungus. If the condition progresses undetected for merely several days the fatality rate can soar to 50 percent. Ward after ward in the Seven Star Hospital in Nagpur is crowded with patients who had recovered from COVID-19, but despite having been healthy before COVID onset, were struck by mucormycosis symptoms.
Labels: Delta Variant Virus, Diabetes, India, Mucormycosis, Post-COVID Infection

0 Comments:
Post a Comment
<< Home