Science Searching for Solutions
"Despite virtually 100% documented one-dose coverage in some regions, large outbreaks of measles involving thousands of cases persisted ... Clearly, because of primary vaccine failure; Canada's one-dose program was insufficient."
Measles Elimination in Canada; 2004 report by Canadian government officials
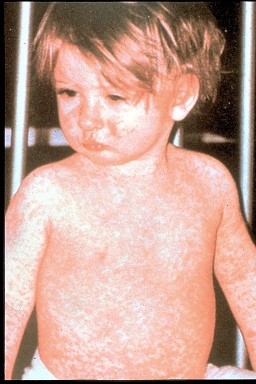
Most people think of measles as a benign childhood affliction. Children get it and then they get over it. And that was well before the advent of vaccination against measles. But in the early 1900s, as hard to believe as it may seem, measles was responsible for the death of millions of people annually around the globe. Until in the developed world at least the death rate dropped by 98% by the 1960s.
Scientists are in general agreement that the decline in measles-caused mortality could be traced to improved health care, better nutrition and perhaps hygiene advances. Perhaps no small part of that was that those who were infected with measles and suffered no lasting ill effects comprised a demographic invested with naturally-caused immunization, preventing them as adults from measles infection.
Measles is hardest on the very young and the mature; lifetime immunity resulted from measles exposure. When a measles epidemic swept through the young of any population there was the assurance that as adults they would not become re-infected through that lifetime immunity left by the original infection.
Once a vaccine was discovered and introduced, the death rate from measles continued to drop in the 1970s. Some medical scientists believe the vaccine to have played a minor role in the continued drop citing statistics that pointed out a waning of most infectious diseases during the 20th century, using scarlet fever as an example for which vaccines were never developed.
A century earlier in the United States alone, ten people per 100,000 died from measles infection; by the time vaccines came into use in the mid-1960s, that death rate had dropped to 1/5 of one person affected morbidly. One high-risk obstacle stood out in studies relating to those most highly deleteriously affected: poverty.
In the study Measles mortality in the United States 1972-75, published in the American Journal of Public Health, the death rate from measles was found to be nearly ten times higher among the poor than among families whose income placed them in the lower middle class. Outside metropolitan areas where available health care was the norm, the death rate was three times that of the inner core.
Children with chronic health conditions; compromised health for any reason; were afflicted by the measles virus disproportionately to the balance of the child population. Fifty years ago, Roger Baskin, with the Center for Disease Control recommended that because of their vulnerability, poor black children and children "physically or mentally retarded, or both" be targeted for measles vaccination in recognition of their greater susceptibility.
During the current vaccine era, adults account for one-quarter to one-half of measles cases, where pneumonia and hospitalization are often-experienced outcomes. Expectant mothers who have been vaccinated remain at risk because the measles vaccine wanes with time, and, sadly it often fails to protect against the very virus it was meant to resist.
Studies from the United States and Japan of pregnant women who had measles found linked occurrences of mother mortality, pneumonia, hepatitis, premature labour, and spontaneous abortion or still births. In other instances babies were born with congenital measles, and hemorrhagic shock and pneumonia plagued a few of the mothers studied. Of a group of 58 mothers studied in Los Angeles, 35 of the mothers were hospitalized; 15 contracted pneumonia, two died.
Babies' bodies are not robust enough to receive measles vaccination until they reached a year of age. Infants suffer the highest rate of measles infections and potentially the most lasting harm in their first year of life. Infants born to women who have been vaccinated receive few antibodies from their mothers, while mothers protected by natural measles have an advantage until three months of age.
The early measles vaccines had indifferent results, sometimes seriously dangerous results. By 1970 Canada and the United States withdrew one of the two original vaccines after it was seen to cause atypical measles syndrome resulting in high rates of pneumonia. Five years later the second original vaccine was taken out of use as a result of the high fevers it encouraged.
The problems appeared irresolvable until the obvious occurred; adding a second dose for children. It worked very well, then that protocol too saw its effectiveness wane. Experts are now recommending reforms; earlier child vaccinations, and second-dose regimens for adults. But a reliable solution has yet to present itself to the larger picture of measles prevention.

It is a puzzle wide open to further study. In the meanwhile, public health authorities urge parents of young children to ensure their inoculations are up to date for all the childhood diseases that present as avoidable, and when children enter the school system they are required to present medical documentation attesting to the fact that their children have received all the required inoculations.
Unless they have been exempted for complicating health factors, religious objections, or other reasons deemed acceptable by authorities. The goal is to obtain sufficient coverage of virus-resistant children through 'group-immunity' to prevent outbreaks compromising the health and safety of the greater population.
Labels: Family, Health, Medicine, Social Welfare


0 Comments:
Post a Comment
<< Home