Preventing Suicide when the Patient is a Doctor
"The impact is huge when we hear of a student or another physician committing suicide."
"Although we don't know the actual circumstances around this particular tragedy [the most recent suicide by a medical student at University of Ottawa], I think we do understand what is happening in the profession itself where there is growing concern over how much burnout we are seeing and lots of depression and suicidal ideation."
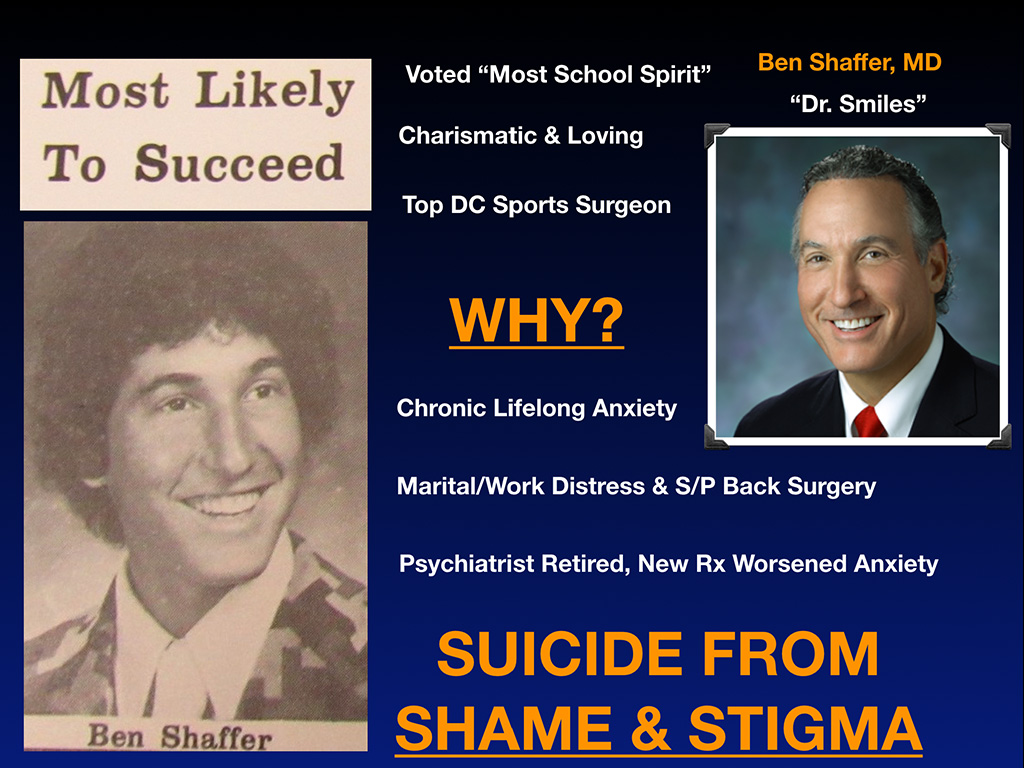
"[There has to be a cultural shift within medicine from a] shame and blame culture that pushes you until you just don't know anymore. If you admit failure or a mistake, it is considered weakness."
"I believe it is time to open a national conversation about it. To face it. I believe we have to create an environment of psychological safety to get the best care for patients."
Dr.Sandy Buchman, president, Canadian Medical Association
"Any time anything like this happens, it is really difficult for the medical community as a whole. We have heard too many cases."
"All medical faculties have been working very hard and recognizing it is an issue, but there is still a long way to go in terms of stigma and learning environment pressures."
"Overall, we know the trend in medicine is that a lot of people are struggling. [There is] still a lot of work to do in the area of destigmatizing mental health in medicine."
Dr.Victor Do, president, Canadian Federation of Medical Students
"[Culprits? How about medical schools perpetuating a culture that becomes ingrained — one where] powering through [consecutive work shifts means you've arrived]."
"These people who have been previously abused are now the teachers. They're teaching the next generation of doctors."
"I know a lot of them [doctors who must seek psychiatric treatment without jeopardizing their medical licenses.] They're having to sneak out of town, pay cash and use a fake name to do it. Why are we putting these people in such a situation?"
Dr.Pam Wible, family practitioner, Eugene, Ore
 |
| CDC: U.S. Suicide Rates Have Climbed Dramatically |
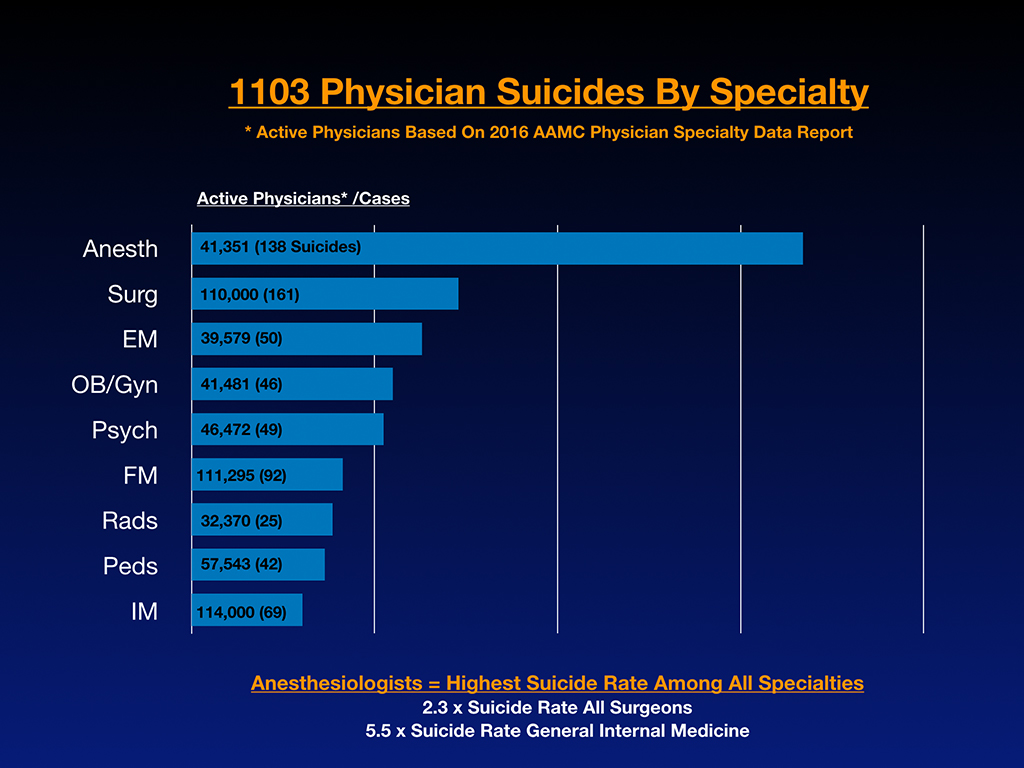
In the United States an estimated 300 to 400 doctors commit suicide annually, representing a suicide rate of 28 to 40 per 100,000. That is over twice the rate of suicide seen in the general population, according to a mega review; a study of ten years of literature on the subject presented several years back at an annual meeting of the American Psychiatry Association.
Last year's survey by the Canadian Medical Association highlighted high rates of depression and burnout among doctors, with an especial emphasis on residents and female physicians. A student doctor who had recently committed suicide had been known for his work toward destigmatizing mental-health issues in the medical profession, where a student who admits to depression and concerns over mental illness may jeopardize their medical career.
"The concerns here mirror those in the United States. We've known for a number of decades that physicians have a higher risk of attempted and completed suicide."
"One of the unique things about Canada is we have a lengthy history of trying to reach out and support doctors right from the very beginning of their careers to try to prevent such tragedies."
"[Although doctors face the same challenges in their personal lives as average Canadians], they've also chosen to work in a part of our society that is full of pain and tragedy."
"Often, we're the ones, like other health care professionals, who witness and contain incredible amounts of trauma, loss – some things that are truly horrific."
"So there are a number of workplace factors. And again we're like every other human in the country: we're vulnerable to things like depression, anxiety, substance use."
Dr. Derek Puddester, associate medical director, Ontario Medical Association’s Physician Health Program
 |
According to statistics, doctors kill themselves at rates significantly higher than what occurs in the general population. For female physicians the risk of suicide is two to three times greater than for women in other professions, and for male doctors the risk is twice as high as males in the general population. Research points to Canadian medical students struggling with pressure, depression, mental health issues, diagnosed with mood and anxiety disorders and psychological distress at levels in excess of the general population.
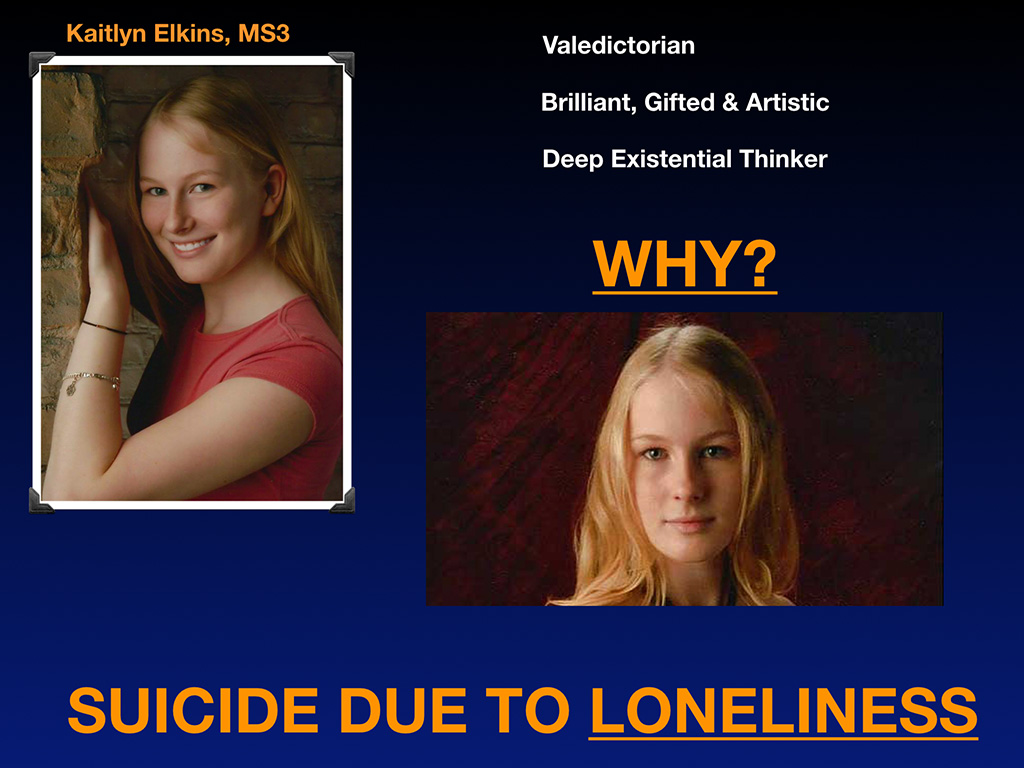
Published in the Journal of the Association of American Medical Colleges, the survey pointed out suicidal ideation among medical students is higher than average. The faculty of medicine at University of Ottawa posted a note on social media referring to the young male medical student whose suicide shocked the profession, as "a caring, positive individual, always smiling and ready to help his fellow students learn", whose death "leaves a hole in the hearts of all those who knew him." That description and that horribly sad end has its counterparts in previous such events of suicide among medical practitioners.
 |
The high-pressure environment of medical school often leads to those who pass the academic bar for entry, to nurse perfectionist tendencies and to submit to chronic self-criticism. When there are occasions of failure resulting from work-exhausted professionals making errors that result in patient harm, the doctor involved can be the most self-blaming, haunted by the event, leaving them with the burden of feeling responsibility to the extent they become virtually incapable functioning, ending up being driven to despair and suicide.
The culture of perfectionism linked with caring for patients who are extremely ill and totally dependent on the professional skill of doctors takes its toll. Medicine is not a risk-taking profession. The assurance of a medical procedure such as a surgery is that the surgeon is a skilled professional with years of experience behind them, and when events go awry as they can, a surgeon can feel overwhelmed and incapable of carrying on. The spectre of medical lawsuits, of reputational damage, of guilt-induced feelings of failure can all singly and collectively destroy confidence and mental stability.
Stigma is a difficult burden to overcome, to convince the medical community that its practitioners are only human and as such require the support of their peers and their overseers. As long as a confession by a medical professional of uncertainty and fear, of unease in their capability to perform and a need for counselling and care is seen as professional failure, driving that individual to submerge those fears and allow depression to fester and mental health to disintegrate, suicide will appear as a 'way out' of the dilemma they face.
The Canadian Medical Association produced a brief general impression of physician attitudes to the profession based on a survey, which discovered that almost a third of surveyed respondents had experienced burnout, even while those within the group reported high emotional, psychological and social well-being.
Labels: Depression, Medical Professionals, Medicine, Mental Health, Suicide

0 Comments:
Post a Comment
<< Home