Sex and Unanticipated Consequences
"This is a cross-continent thing we've been observing over the past number of years."
Dr.Chris Sikora, medical officer of health, Alberta
"Each part of Canada is kind of experiencing its own version of the epidemic. Unfortunately, we have effective testing .. and yet we still have an epidemic."
"There's no reason why it shouldn't be able to go away."
"It's not very nimble [lack of data, reliance on test reports] in terms of understanding what's shifting on the ground."
"If people are only peeing in a cup then they're not getting tested for syphilis. We cannot let our foot off the gas in terms of managing this."
Nathan Lachowsky, public health professor, University of Victoria
"In the initial part of this outbreak, many of the cases ... were among gay and bisexual men. In the last two years or so there's been a definite shift to heterosexual persons."
"Meth is a very important component of what is happening."
"A recent rise in the use of smartphone-based dating applications, which make it easier to meet sex partners, has been linked to increased likelihood of risky sexual behaviours among people of all sexual orientations."
Dr. Ameet Singh, clinical professor, division of infectious diseases, University of Alberta
 |
| Patrick O'Byrne, a nurse practitioner at the Ottawa Public Health sexual health clinic, says syphilis is known as the great masquerader because it can look like other illnesses and can be so difficult to diagnose. |
Syphilis is making a comeback worldwide, and it is hitting some areas of Canada particularly hard. Syphilis has been known through historical accounts as a disease that struck some notable personages. It was also known by its ravages as a disease associated with facial deformities and dementia, left untreated. In 18th-century England one city had syphilis striking up to eight percent of its population. The first outbreak of syphilis was reported in 1495, when Naples was sacked by the French army.
Interestingly enough, 1492 was when Christopher Columbus sailed to the Americas. Theory has it that soldiers with the Columbus expedition picked up the infection on the voyage, bringing it back to Europe. This competes with another theory that it already existed in the Old World, but was mistaken from another dread disease that left people mutilated -- and where colonies were instituted to shut these outcasts away from society -- suffering from leprosy.
 |
At the turn of the Twentieth Century, people went so far as to deliberately expose themselves to malaria hoping to fight syphilis, thinking that high fevers typical of malaria would extinguish syphilis symptoms, and malaria itself would be cured with the drug quinine. A treatment prior to that saw mercury applied to the skin, or fumigating people with mercury. The world of medicine now responds to treating syphilis with antibiotics. Nothing quite beats prevention and regular testing, however.
This, for a dread disease held to have been eliminated as a health and longevity threat, eliminated as far as the medical community was concerned in the 1990s in Canada. Syphilis when it first presents looks like a sore on the mouth, genitals and anus, a painless nuisance until the symptoms progressively worsen. Without treatment, lying dormant for years, it can be the cause of brain, nerves, eyes, heart, blood vessels, liver, bones and joints damage.
In Canada, the most recent data indicate 6,311 cases of syphilis in 2018, an increase from the 2,399 registered in 2014, according to a report released in November by the Public Health Agency of Canada. The highest rates are seen in 30- to 39-year-olds, with per capita numbers illustrating an enormous swing from 234 cases per 100,000 people in Nunavut, to 2.5 cases in New Brunswick, per 100,000, and with the national average around 11 cases per 100,000.
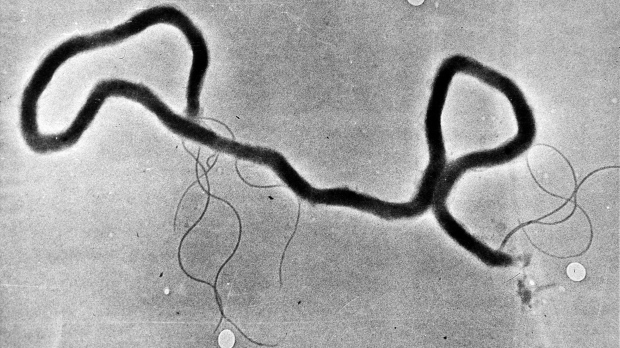 |
| Treponema pallidum, which causes syphilis, through an electron microscope. AP |
The Province of Alberta has seen a large increase in reported cases, with 1,536 in 2018, an increase of 187 percent from the previous year. In 2019, 1,753 new diagnoses were made compared with a mere 151 in 2014. Its rapid spread is of great concern among specialists in the medical community. Moreover, lack of associated data make it difficult to fully understand the contagion, with researchers relying on test reports which lag in time and offer no insights into the non-tested community.
A troubling offshoot of this trend is the emergence of a rise in congenital syphilis, of children born with the infection. Across the country, 17 confirmed cases of congenital syphilis -- the highest rate in 25 years -- were reported across the country, according to the Public Health Agency of Canada. Alberta alone has seen 38 cases of congenital syphilis in 2019.
Dr. Singh of University of Alberta attributes a few factors to this rise; one of which is the use of methamphetamines, the use of which stimulates sex drive and is associated with risky sexual behaviours. Casual sex and multiple sex partners attributable to shifting cultural values and the availability of dating apps are all viewed as possible contributing agents to the rise and spread of this highly communicable disease. Added to which increasing numbers could be linked as well to more frequent testing through blood tests.
 |
| Earliest known medical illustration of syphilis, Vienna, 1498 |
HIV pre-exposure prophylaxis which can prevent HIV infection, led to a reduction in condom use among men who share sex with other men, a practise which pushed sexually transmitted infection (STI) rates higher.
An initiative has been undertaken by the federal government through a five-year action plan to focus on STIs and blood-borne illnesses, including syphilis, HIV/AIDs and hepatitis C in hopes of reducing rates and improving access to treatment and testing.
The rising numbers can be curbed through prevention and regular testing. Annual tests are urged upon people whose sexual behaviour places them at increased risk for contracting syphilis.
Labels: Contagion, Epidemic, Health, Syphilis, Tests, Treatment

0 Comments:
Post a Comment
<< Home