Choices in Life and Death : Organ Transplants
"Amnesty International, in an open letter to Health Minister Dr. Eric Hoskins and Trillium Gift of Life president and CEO Ronnie Gavsie, asserted that 'To deny individuals access to necessary and life-saving medical treatment purely on the grounds of their prior or current health status -- including conditions resulting from the use of alcohol -- is discriminatory."
"There are many factors that go into the decision as to who gets on the waiting list, and who indeed receives an available organ. No one, not the governor general, the prime minister or provincial premiers, for example, can jump ahead."
"Ethnicity, gender and race are never, I repeat, never, a factor. Amnesty International's allegation of discrimination is preposterous, unfounded, unfair and irresponsible."
"When it comes to organ allocation, the criteria are clear, and up to this point in time, universally accepted. There is no moral judgment at work in this process. The greater chance for recovery is a definite factor in the deciding process."
Rabbi Dr. Reuven P. Bulka, C.M., chair, board of directors, Trillium Gift of Life Network, Ontario
"I'm really feeling for the families who have lost loved ones due to these policies, due to small technicalities and things that could have saved so many lives."
"I'm not completely out of the woods after this [her gradual recovery through therapy other than a liver transplant]. The staff here [University Health Network, Toronto] have been amazing. Same as Ottawa General [hospital]."
"The uncertainty of whether or not I need a liver or if I would get a liver — that scares me. I'm not ready to die."
"It's unfortunate there are policies that could have found me in a different fate. My next step is to see [a hepatologist] and see what damage has been done for the long term."
Delilah Saunders, 26, Inuk woman from Ottawa
 |
| Delilah Saunders in her Toronto hospital room on Tuesday. The 26-year-old activist was told two weeks ago she needs a new liver, but is ineligible for a transplant because of her recent drinking. (CBC ) |
Aboriginals are known to be susceptible to alcoholism, it has always been a problem and continues to be a problem, a reality that cannot have been unknown to Ms. Saunders and her family. Alcohol consumption is a considered and deliberate choice; no one is forced to drink liquor. That choice led to the situation in which Ms. Saunders found herself recently; the reality that transplant material is in short supply necessitating that what is available is carefully husbanded. The point being transplant organs ideally should be used when those receiving them have a commitment to their own care.
That being the case, when someone has a history of alcoholism and then suffers the consequences in liver failure, they will not -- and this is indeed a universal concept -- be placed on a list of recipients awaiting transplantation until such time as they can demonstrate that they have refrained from drinking for six months previous to their application. Organ donations are in short supply, so much so that in Ontario in 2015, 127 people on a waiting list died while awaiting a transplant. That being the case what kind of common good sense would it be to transplant someone who is an alcoholic?
According to Dr. Nazia Selzner, a transplant liver specialist in the multi-organ transplant program at the University Health Network in Toronto, a wide variation in the rate of relapse to alcoholism after transplant is a reality. Studies, according to Dr. Selzner, vary between ten percent of patients relapsing, up to "as high as 90 percent".
A long-term study that saw publication in the American Journal of Transplantation in 2010 found that roughly 40 percent of the 208 patients with alcohol-related liver disease whose cases were studied over a number of years, had relapsed into heavy drinking. This is the issue, and it is one of careful use of a rare resource for the best possible outcome to society when people in need of a transplant can wait for years until that opportunity arises.
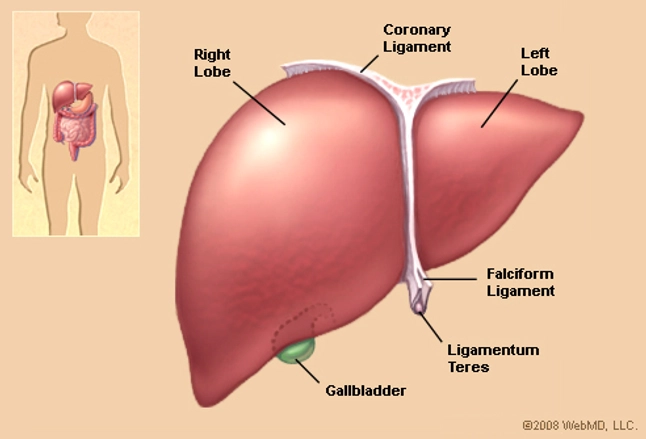
The over-heated charge by Alex Neve of the Canadian branch of Amnesty International along with Aboriginal groups that Indigenous people are deliberately excluded and victimized is slanderous and just plain wrong. These two groups have gone public in hysterical accusations in an effort to incite public indignation over yet another perceived wrong done to Canada's Aboriginal population. The argument that the existing policy is discriminatory, harming the poor, the marginalized and Indigenous is a charge void of accuracy.A liver transplant is done to treat liver failure, which can have many causes, including chronic hepatitis B or C, fatty liver disease, alcoholism, and autoimmune liver disease. A donated liver can come from a living donor, who gets part of his or her liver removed, or a deceased donor.
Typical costs:
- For patients covered by health insurance, out-of-pocket costs for a liver transplant typically consist of doctor visit, lab and prescription drug copays as well as coinsurance of 10%-50% for surgery and other procedures, which can easily reach the yearly out-of-pocket maximum. Health insurance will typically cover a liver transplant.
- For patients not covered by health insurance, a liver transplant typically costs up to $575,000 or more for the procedure, including follow-up care and medications for the first six months after the procedure.
- According to Vimo.com, a health care cost comparison website, the average list price for a liver transplant is about $330,000, while the average negotiated price, through an insurance company, is $100,400 U.S. Figures
Ontario's donor agency is contemplating a pilot project to waive the six-month sobriety requirement for heavy drinkers requiring liver transplants. "Our goal is to start it as early as possible, which means accelerate the planning of the pilot and the resources required to support it", explained Ronnie Gavsie, chief executive of the Ontario's organ donation agency, Trillium. "The way we're going to win here is if all of us, every one of us who is 16 years of age or older, register consent at beadonor.ca."
Labels: Alcoholism, Bioscience, Controversy, Health, Organ Transplants

0 Comments:
Post a Comment
<< Home