The Anguish and the Agony
 |
| The spread of COVID-19 ramps up. (Ben Nelms/CBC) |
"In the next two weeks, that's when we're really going to start feeling that [burnt-out] in our hospitals. We are very worried. We're terrified.""It 's inevitable it's going to happen and we just need to brace ourselves for it [a COVID 'third wave'].""Let's say the ICU is full. That's a real risk right now. How do you make the choice about which person deserves a ventilator or an ICU bed more [than another patient]?"Dr.Shazma Mithani, emergency room doctor, Edmonton, Alberta"We're all really, really scared about what the next -- not even just the next couple weeks, it's the next few days -- we know that ICU numbers can increase by leaps and bounds in a matter of hours.""We don't know if we're going to be able to keep up tomorrow or the next day, forget the next couple of weeks.""Everyone is just extra tense, extra nervous.""[With workers off sick or caring for family, or resulting from virus exposure, the] pool of nurses is getting smaller and smaller."Edmonton emergency room nurse, name withheld"It's so busy. this is the forgotten part of the pandemic.""When we talk about burnout, it's because we are really being called to go above and beyond what we would naturally do in our general family practice.""I'm really tired, I'm really, really tired ... we're just at the early stages of this wave."Dr.Christine Gibson, Calgary family doctor
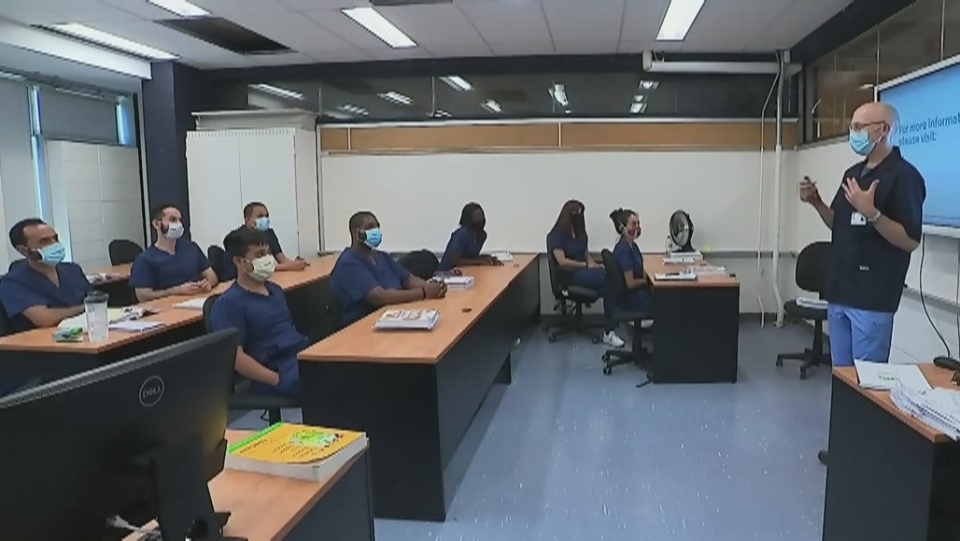 |
| Quebec Orderlies train on the job CTV News |
Canada has seen the number of COVID-19 cases sweep past 344,000 with deaths linked to the coronavirus over 11,600 in number leaving medical workers fearful of the health system breaking down. They also worry that while treating patients with COVID they are exposed to the virus; will they become ill, will they bring the virus back home with them? Who will look after their family if they're ill? For that matter, who will be left to look after patients' needs, if health workers continue to succumb to the virus?
Even now, staff shortages bedevil the system resulting in part from nurses and orderlies becoming ill. Burnout and illness continue to sideline medical workers right across Canada. This second wave that has inundated the country has taken its toll, and even while it has not yet reached an anticipated crescendo, fears of a third wave haunt the health community. Health care workers are doing double duty given the growing shortage of workers and they're exhausted.
Doctors like Shazma Mithani feel Alberta's government has failed to bring in sufficiently stern legislation, leaving people free to gather indoors at places of worship, in bars, casinos and restaurants. Contact tracing has broken down while up to 80 percent of cases are without data to show where they were contracted. COVID-related hospital occupancy and ICUs across the country both on the rise in an already difficult situation where most hospitals have reached their capacity.
 |
| ‘This is the most scared I’ve seen people in my 27 years as a nurse.’ BC’s health care workers are doing their best to find relief. Photo by Joshua Berson |
Two days ago Ontario had 523 people in hospital, 159 of those in ICU, while in British Columbia 284 people were in hospital, 61 in ICU. "It becomes a daily struggle to find the right place to care for people and the right tools to apply your knowledge well", remarked Dr.Kevin Smith, president and CEO, University Health Network, Toronto. Hospital staff fear longer wait times in crowded hospitals will result in worsening health outcomes for their patients.
The first wave in the spring presented a problem of shortage of protective gear and medical supplies, along with hospital beds, whereas this second wave threatens outcomes through a shortage of trained medical personnel. Demands of the pandemic has led to 'moral distress' for health workers. "When you can't provide the quality of care that you have in the past, it becomes that much harder to tell yourself you're doing a good job", explained Lonee Rousseau, a registered nurse, and vice-president of the union local at Royal Alexandra Hospital in Edmonton.
In Steinbach, Manitoba, nurses point out that patients are now forced to wait in their cars as a result of insufficient hospital space, calling out for more staff in a province that has recently seen its case load explode. Over 3,200 health-care workers in Alberta alone have been infected by COVID-19. According to data published by the Ontario government, over 8,400 health-care workers ranging from dentistry to first-responders, to respiratory therapists, to personal care workers, have contracted COVID-19 since spring.
 |
| Care workers are ‘constantly on edge waiting for the next step and reflecting on the last step,’ says Dr. Ed Marquis of Prince George. Photo by Joshua Berson |
"The fear right now is that this is only getting worse and so there's an anticipation, a dread anticipation, going on within our system.""We really need to see people when they're sick. There was this mortality bump [in May and June] ... basically due to people putting off hospital visits for illnesses when they should've [come in].""And that [seeing two COVID-19 deaths recently] may seem like, whatever, you're an emerg.doc, you see death.""But this is different. And so fast. And we just know that it's going to get worse."Dr.Joe Vipond, emergency room doctor, Calgary
Labels: Burn-out, Canada, Global Pandemic, Health-Care Workers, Increasing COVID Cases, Medical Personnel, Shortages

0 Comments:
Post a Comment
<< Home