Hope for the Future of Cancer Treatment
"The cancer was just melting away. Today I find out I'm in full remission -- how wonderful is that?"
"This is the hope of any cancer patient, that if you stay in the game long enough, the next treatment's going to be just around the corner."
Ken Shefveland, lymphoma patient, Vancouver, Washington
"We're talking, really, patients who have no other options, and we're seeing tumours and leukemias disappear over weeks."
"[But] there's still lots to learn [about cellular immunotherapy: CAR-T cells]."
Dr. Stanley Riddell, immunotherapy scientific director, Fred Hutchinson Cancer Research Center
"It shows the unbelievable power of your immune system."
Dr. David Maloney, medical director, cellular immunotherapy, Fred Hutchinson Cancer Research Center
"We can essentially make a cell do things it wasn't programmed to do naturally."
"Your imagination can run wild with how you can engineer cells to function better."
Dr. Philip Greenberg, immunology chief, Seattle immunotherapy clinic

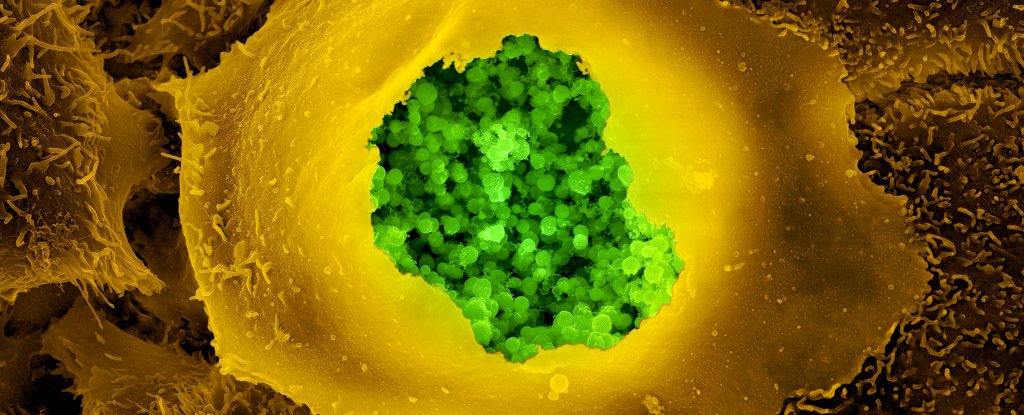
Early studies in the United States saw 60 to 90 percent of patients whose last-resort attempts as trial patients for leukemia or lymphoma, experiencing the profound relief of seeing their cancer decrease or even become undetectable, in fairly short order after trying experimental CAR-Ts. T-cells are the warriors of the body's immune system, they are geared to attack deranged cells. Even so, they often miss cancer cells, stopping immune attacks.
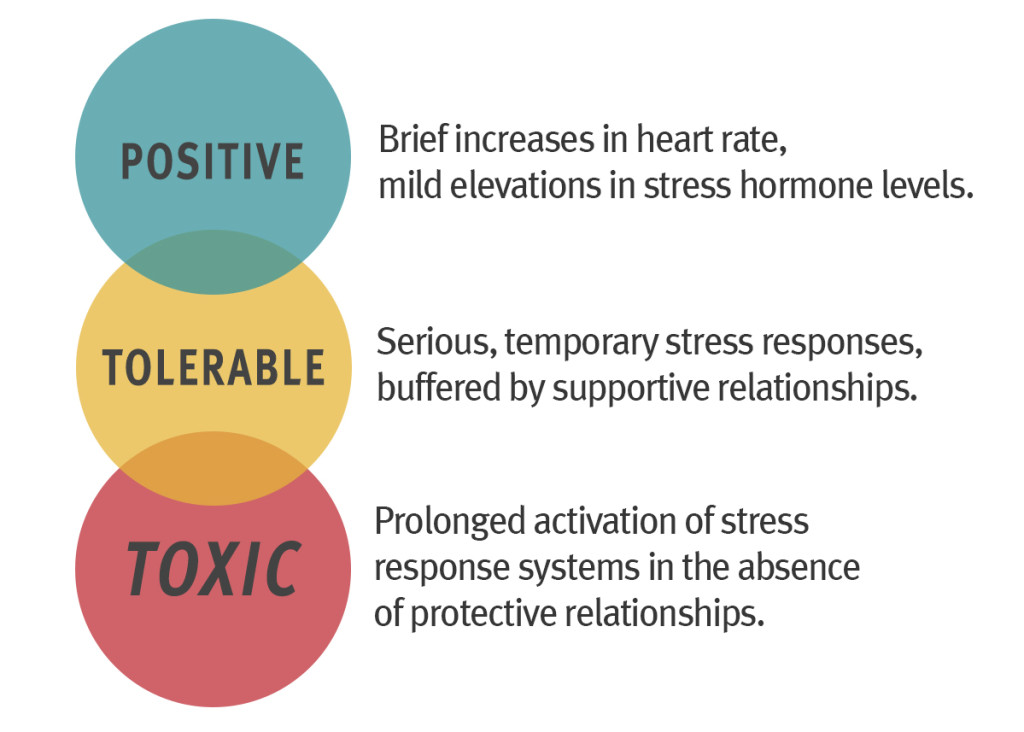
But the increasingly promising immunotherapy drugs named "checkpoint inhibitors" have the purpose of releasing a brake that T-cells place on an immune attack to protect the body from cancer cells. This new cellular immunotherapy process is purposed to become more powerful, allowing the patients' T-cells to become stronger and more functionally responsive to invasion by deranged cells.
The process remains in its experimental stages, where volunteer patients who no longer have much to lose because their cancer has become so devastatingly deadly and impossible to bring to a halt by any other means, take part in CAR-T cell therapies. The reaction to their use has been so encouraging that the therapies are now being evaluated in two different versions by the US. Food and Drug Administration for eventual use in hospital settings.
Scientists are not, however, sitting back on their heels in self-congratulation. This is the first major step in fighting cancer, and following steps are pressing at their heels. "The acid test" of the new immunotherapy is to determine how it could be successfully used to target common cancers where solid tumours attack lungs, breasts or appear as brain cancer. Cancers of various types kill some 600,000 Americans and 79,000 Canadians annually.
Another testy concern is that living cancer drugs such as are represented by these new therapies are effective in some people, and not so in others. Potentially life-threatening side-effects when the immune system is overstimulated as it is with the CAR-T process, occur in some patients and in a small number, deaths from brain swelling can occur. "It's a Model A Ford and we need a Lamborghini", stated Dr. Renier Brentjens of New York Memorial Sloan Kettering Cancer Center.

For 67-year-old leukemia patient Claude Bannick, the experience with a CAR-T study in 2014 was a positive one for a man whom chemotherapy, experimental drugs and a bone-marrow transplant had all failed. A machine filtered out his white blood cells containing T Cells, then his cells were raced to a facility to be reprogrammed. After his 14-day ordeal of suspenseful waiting, he now says that CAR-T is "giving me a second life".
CAR-Ts kill some healthy white blood cells because they cannot yet be completely accurate in identifying their targets. Along with cancerous cells some B cells are destroyed since both contain the same marker; yet another complication. An immune overreaction named "cytokine release syndrome" when CAR-T cells surround cancer cells can trigger high fevers and falling blood pressure where in severe cases organ damage may ensue.
This completely novel way to treat cancer holds immense promise, in the hope that scientists can successfully tweak it to work more safely. One-time infusions of supercharged immune cells have helped an astonishing number of patients suffering from leukemia or lymphoma, at their intractable stage, when nothing else gave them hope for the future. But another concern looms in that it is an unknown how long the cancer-cell responses will last.
According to the findings of a recent review of the therapy and its aftermath, it is expected that up to half of leukemia and lymphoma patients may ultimately suffer a relapse.

Labels: Bioscience, Cancer, Medicine, Research, Therapy