Treatment of Pain Leading to Death
"Some have suggested that [pressure from pharmaceutical industry for use of opioids in chronic pain treatment] may be one of the reasons behind it [heavy opioid use in North America] -- like anything else, it is multisectoral."
"I think it is something we do need to ask ourselves and I think that part of answering that ... is where we are going to find some of the clues as to how we respond."
"People need to have access to these effective medications where used appropriately, but there is tremendous risk potential. People do become addicted to them and people die."
"It affects health-care providers, it affects organizations that represent people who use drugs or have used drugs and their family members ... we need [the] research community on board, we need community associations on board."
"There's a very wide range of organizations that need to be involved in order to address the problem from the point of view of prevention [of opioid abuse] and [pain] treatment."
Health Minister Jane Philpott, Canada

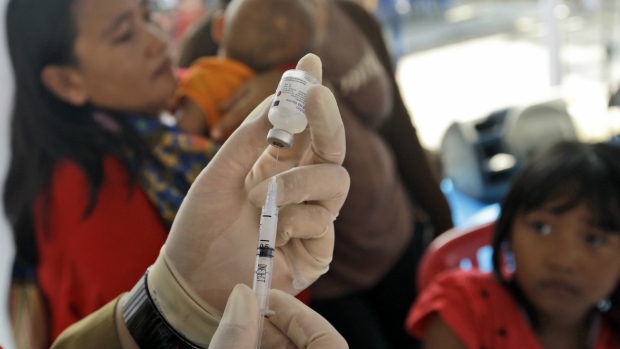
Physician and Cabinet minister Jane Philpott is applying herself to the conundrum within the medical community of prescribing painkillers to patients suffering pain and discomfort, and through alleviating their pain, risking drug addiction, overdoses and death. The pharmaceutical industry plays no small part in this viciously revolving scenario of prescription drugs presenting as a threat to the patient community in Canada; a situation reflected in the United States.
Traditional extensive lobbying of doctors and hospitals to influence the trusted use and over-prescription of opioids has long been an issue awaiting urgent attention. Oxycodone, fentanul and morphine and illegal street drugs like heroin are creating an epidemic of addiction and increasingly, drug overdoses. In some quarters a level of control is seen through the use of a nasal spray whose impact is designed to reverse or halt the effects of overdoses.
The naloxone hydrochloride contained in the spray is a recognized medication that has the potential to save lives. While currently available in Canada in an injectable form, Health Canada has recently stepped forward to ensure it could be available as an antidote to overdoses without a prescription in the instances of emergencies occurring outside hospitals "I think that from an international perspective, that's considered to be very good practice, and I'm absolutely convinced that many lives will be saved."
British Columbia has declared a public health emergency, responding to a steep rise in fatal drug overdoses overwhelming the province. In January alone an estimated 74 overdose deaths occurred in British Columbia, on track to exceed the 474 deaths from drug overdoses that struck the province in 2015. And as from January 2017 high doses of painkillers are set to be removed from the Ontario Drug Benefit Formulary. That will affect people 65 or older, those who live in long-term care, receive social assistance or incur high drug costs relative to income.
"We're starting to see doctors prescribe them somewhat less regularly, but they are still used very, very often. And, I think, too often", commented Dr. David Juurlink, head of the division of clinical pharmacology and toxicology at Sunnybrook Health Sciences Centre in Toronto, who lauds the Ontario Ministry of Health for the "good move" on its part, which may further persuade physicians not to prescribe unnecessarily high doses of the drugs.
Lower doses of the drugs will not be affected by this initiative. The ministry claims that lower doses can in fact be more effective for the purpose of pain relief than high doses, and without the obvious potential for overdose leading to death. So as far as the Ontario Health Ministry is concerned, delisting high doses represents a step forward.
Provincial prison inmates are 12 times likelier than the general public to die of a drug overdose. Within the first year of their release from prison; 77 percent of sudden, unexpected deaths have been attributed to opioids. The thing of it is, as soon as one aspect of a problem appears to be moderately solvable, another arises to make the situation more complex and dangerous.
A drug specifically used to sedate elephants, a hundred times more potent than fentanyl, is now suspected to be present in overdoses in a few states in the U.S. Authorities there believe it is mixed with, or passed off as heroin. One of the most potent opioids known, carfentanil makes the confrontation of the proliferation of overdose deaths more complicated.
In central Ohio a man suspected of selling carfentanil, claiming it to be heroin, was indicted on 10 counts this week. He has been connected with a July 10 death, along with nine other overdoses.
Zoo veterinarians carefully wear face shields, gloves and other gear to protect themselves when preparing carfentanil for use. A single drop splotched into an eye or hose could be fatal, according to the American Association of Zoo veterinarians.















 An
An










