"[Once the virus is cleared, the body's immune activation goes rogue, unleashing auto-antibodies that turn on its own tissues and proteins. Somehow the immune system has become confused and rowdy], and what you're left with is the collateral damage."
"I just kept thinking, I'm a trained immunologist. I know what might be happening to me, and I'm getting this anxious. What's happening to other people who don't know about it."
"We need to find out what exactly is happening. We need to do studies in bigger numbers, in collaborations, over time."
"And the people who are fighting this, who are going through this, need to come and get themselves enrolled in studies and stick to the study so that we can understand this disease."
"Because unless we understand it and see it and report it and be honest about what we are seeing, we'll not be able to get to the bottom of this."
Manali Mukherjee, assistant professor, Department of Medicine, McMaster University
"The long COVID thing, has been slightly overblown, and as soon as you do proper epidemiological studies you find the incidence is much, much lower."
Sir John Bell, immunologist, Regius Professor of Medicine, University of Oxford
"This has been seen post influenza, it's been seen after SARS."
"We have to be really cautious about not under appreciating how chronic and persisting these symptoms can be."
"[Yet there is] absolutely [still skepticism among the medical and scientific community] because we're dealing with a condition that is new."
"Anyone can be impacted by this, young and old alike, and even if you were asymptomatic during initial infection."
"We are dealing with a real entity here."
Dr.Fahad Razak, internist, epidemiologist, St.Michael's Hospital, Toronto

There is disagreement among medical specialist over the appearance and presence and indications of long COVID; some convinced it is real and destructive, others dismissive of it as a bit of patient hysteria. Dr.Mukherjee is in the former group. She has been suffering symptoms associated with long COVID, and as a medical professional has been studying the phenomenon. As a person, she is also someone who was diagnosed in January with COVID-19. Since then she has been struggling with staggering fatigue, sudden plummeting blood pressure and difficulty in focusing "There were good weeks and then there were bad weeks", she explained.
In her incidental capacity as a scientist, she is the recipient of a half-million dollar grant in federal funding to study the syndrome she now suffers from. A condition lacking a prognosis or any kind of treatment, which has afflicted an uncertain number of people. People who describe lungs that feel as though they're packed in flour, brain fog that feels like dementia, and a level of fatigue unlike anything they might have previously imagined, much less experienced.
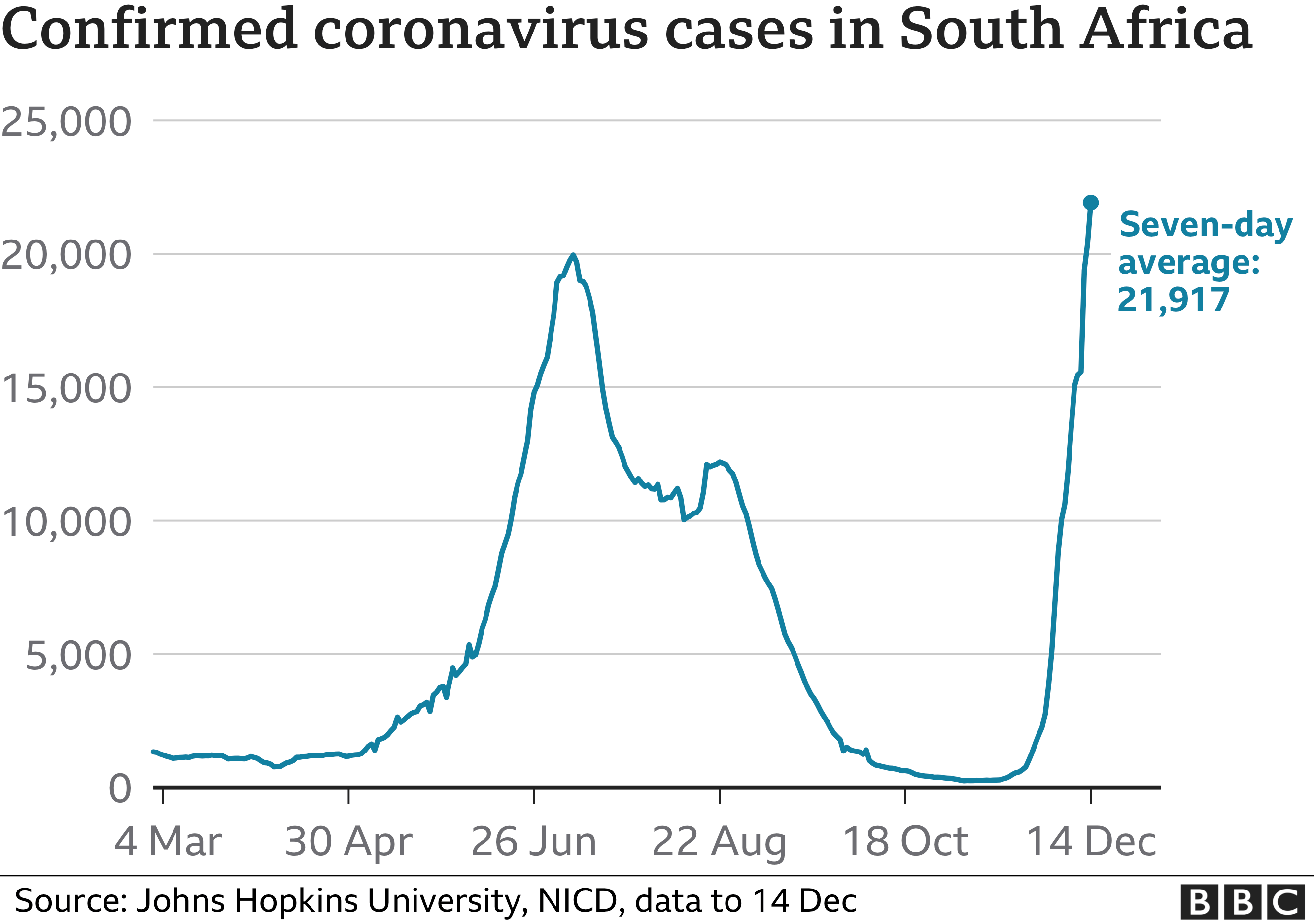
The answer to these symptoms, Dr.Mukherjee believes, is somewhere located in the immune system, a hyper-stimulated immune response once the virus has cleared. World-wide there have been 271 million cases of the SARS-CoV-2 virus infecting people with COVID. According to some researchers, long COVID represents the next "looming Catastrophe", where estimates of prevalence range from two percent of the COVID "recovered", up to 89 percent.
"Long haulers" have identified a world of symptoms affecting close to every organ system in the body. No cause has to this point been proven, even the definition of what it is that defines long COVID "is still very much in evolution", said Steven Phillips, vice-president of science and strategy at the COVID Collaboration. And, he elaborates, while the symptoms are very real "and really seriously afflict people", the problem remains complex, difficult to diagnose and unpredictable.
There are studies published that have found people who report symptoms are sometimes absent evidence of antibodies against SARS-CoV-2. According to the World Health Organization, one in ten people infected with COVID will go on to experience symptoms that go on beyond four months post-COVID. Yet the underlying biological causes are unclear. Post-COVID conditions according to the Public Health Agency of Canada, are defined as one or more symptoms that persist or recur 12 weeks or longer following a COVID diagnosis -- that are not attributable to any other diseases.
Symptoms are wide-ranging, from those most frequently reported -- fatigue, headache and brain fog -- to the more rarely reported such as paranoia. In addition for those experiencing life-threatening infections, spending time in an intensive care unit can acquire life-transforming complications, according to Margaret Herridge, co-leader of a study of one-year outcomes in people infected with COVID.
People who spend a week or longer in an ICU, immobilized and heavily sedated on a ventilator, can experience fatigue, nerve and muscle injury lasting months, as well as cognitive dysfunction affecting memory, attention and problem-solving. An estimated 25 to 35 percent of ICU survivors experience anxiety, depression and PTSD.
"Our data suggest that a full recovery after one year is not possible for some patients, for whom it will take longer to attain their baseline health state before COVID-19", researchers in a Chinese team whose study was published in The Lancet, of COVID hospital survivors infected in Wuhan's first wave which found at a 12-month followup most had returned to work and their normal lives while those with "persisting, severely impaired health status are rare".
Another, French study involving close to 27,000 people whose blood had been screened for antibodies to SARS-CoV-2 found people who believed they had been infected, but whose infection could not be confirmed by the antibody test, were more likely to report symptoms of long COVID. "Beliefs regarding the causes of these symptoms may influence their perception and promote maladaptive health behaviours", wrote the French scientist in their controversial report.
 |
| ‘I had neurological
symptoms early on. Everything felt foggy and far away. I forgot
everything – even things that had happened a few minutes earlier.’ Photograph: Tero Vesalainen/Getty Images/iStockphoto |
"[Over one hundred symptoms have been ascribed to long COVID; the] one most reported, and most debilitating, is terrific cognitive problems, terrific brain fog."
"People say they have absolutely no energy and absolutely no motivation."
"There's a whole neuro-scientific literature now to show that when the immune system is activated it does have a very localized effect on your brain."
"There's no implication this is depression. There is no indication that this is mental illness. We just happen to be repurposing this medication for this very, very difficult to understand condition."
Dr.Roger McIntyre, Toronto psychiatrist
Labels: Long COVID, Research










/https://www.thestar.com/content/dam/thestar/news/city_hall/2021/12/02/omicron-variant-suspected-in-covid-19-outbreak-at-toronto-east-detention-centre/toronto_east.jpg)