The Living Death
"The problem up until now has been that we develop these techniques, we put them out there, we tell people how to do them and the only patients that benefit are the people who make it into other research institutions. It hasn't been incorporated into guidelines for how one treats these patients. And that has now changed."
"[If we can improve prognosis in that group ... brain injuries in the first hours after trauma ,,, if we can better understand who might make some recovery] we can perhaps save some of those lives."
"Maybe a different decision is right for some of those patients [rehabilitation rather than pulling life support]."
"What is most tantalizing about this prospect is that it would allow a seriously brain-injured patient to express their current wishes, which may well have changed radically in the interval before they expressed any premorbid opinion."
"Ultimately, the morally challenging question of whether theirs is a life that is 'worth living' is one that could be answered by the patient using fMRI."
Dr.Adrian Owen, neuroscientist, researcher, University of Western Ontario, London, Ontario
 |
| Neuroscientist Dr. Adrian Owen at the Robart Institute, University of Western Ontario. |
"How reliable is the signal [brain-computer interfaces]? How do we make sure that it's the intent of the person, that it hasn't been hacked and that it is reproducible?"
"It's not good to over-medicate someone but it's much worse to under-medicate."
"[And what good is derived that a loved one seems to have a level of conscious processing, with a scarcity of helping tools?] I think that's where I get stuck."
"The technology has advanced to the point that we must attend to the fact that individuals who we thought were in a persistent vegetative state may not be and, in some cases, certainly are not. And those numbers are bigger than we ever thought."
Dr.Judy Illes, Canada Research Chair, neuroethics, University of British Columbia
Emerging research and statistics now inform the medical community that some twenty percent of people diagnosed as being in a vegetative state, considered to be mentally unconscious, unable to exhibit "willful behaviour", disconnected from cerebral life, in fact really are aware and conscious of what goes on around them, but without the capability to transmit that information, to inform doctors, nurses, medical staff, family members that within that comatose frame remains a brain that is still operational, trapped in a body which it can no longer activate.
British-born researcher Dr. Adrian Owen has been experimenting for years with the use of brain scans with the intention of reaching within the minds of people whom medical science has long considered to be in a mental state of complete nothing, a vacuum in an otherwise-healthy body, de-linked from an inoperative brain. Dr. Owen's objective was to be able to find some way of discovering whether the brain remains quiescently active, and whether some mode of communication could be achieved with someone incapable of speaking or moving.
One of Dr. Owen's patients was a young man who had suffered a catastrophic beating that injured his brain, sending him into the netherworld of disconnected consciousness, 16 years ago, at age 18. The young man from Saskatchewan had a father who refused to believe there was no hope for his son. Which led Paul Tremblay to arrange for Dr. Owen to examine his son Jeffrey whom he flew to London with. The functional magnetic resonance imaging scanner showed Dr. Owen that Jeffrey's brain exhibited electrical activity in the frontal and parietal regions, just as any normal person would.
 |
| Paul and Jeffrey Tremblay Photo courtesy Tremblay family |
Dr.Owen and his research team wrote up their study and had it published in the journal
PNAS, noting that his patient had indicated no "higher-order" signs of awareness. Yet he was exhibiting executive processing, engaging in
"complex thoughts about real-world events unfolding over time", as the experiment with the fMRI indicated. That was six years ago. Since then the scientist at Western University has used fMRI to re-diagnose people once held to be "vegetative", and to communicate with them through elemental responses to questions such as
"are you in pain?", through decoding brain activity.
Now, years later there are bedside EEG machines with small discs placed on the scalp to measure brain activity, moving closer to routine use with catastrophic brain injuries. A recommendation was issued in new guidelines from the American Academy of Neurology that where there is any ambiguity of "inconclusive" findings, brain imaging should be used to hunt for emerging signs of consciousness in the brain-injured, left without recourse to speech or action; a "milestone" development in the history of brain science, wrote Dr.Owen and colleagues in a paper titled "
Alive Inside", published in the journal
Bioethics.
Dr. Owen feels the optimum time for tests is in the first hours after a traumatic brain injury, with a view to predict which patients might recover from a vegetative state, and which might represent a candidate for rehabilitation, and that these tests be widely adopted. This, in the face of the reality that most decisions whether to remove life support happen to take place within the first 72 hours following injury. Other neurologists are now testing deep brain stimulation in hopes of being able to "Re-awaken" or incite awareness in those in minimally conscious states, including years after their injury.
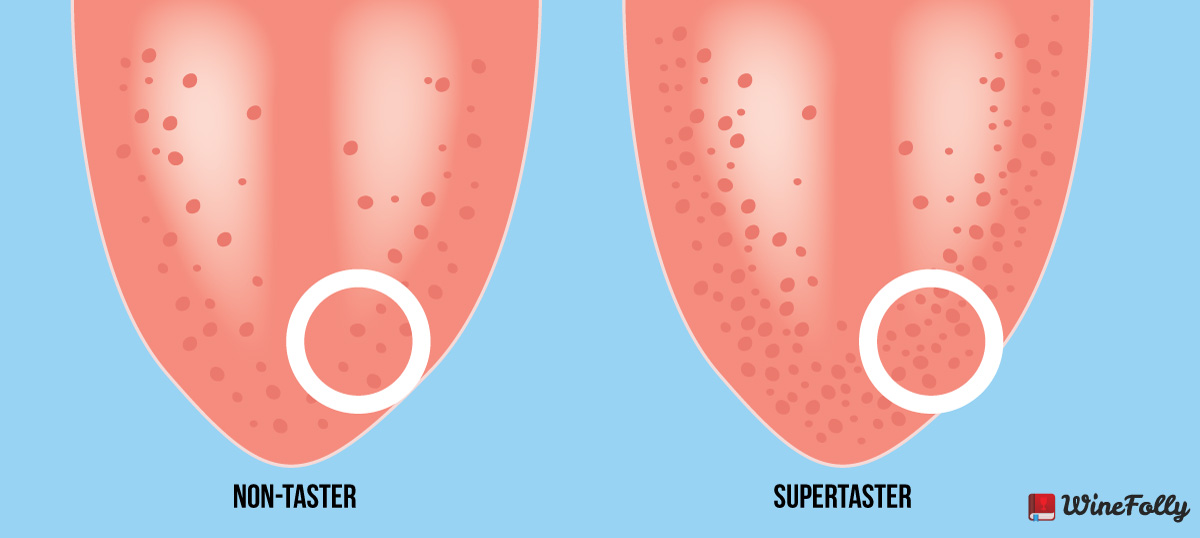
At the present time what has become standard in checking for "residual" or preserved awareness or cognitive function in brains that a stroke, cardiac arrest or blow to the cranium is the use of bedside scales using response and command-following tasks, such as
look this way, squeeze my hand, move a foot, follow the ball with your eyes. What complicates the issue is that people who have been diagnosed in a vegetative state or the larger group falling in the minimally conscious bracket, are unable to marshal physical reactions to blink an eye or move a foot on command; their central nervous system has suffered a disconnect preventing them from any movement whatever even though their mental processes could be intact.
In a later experiment, Dr.Owen and a colleague from the University of Liege, slide a man from Sarnia, Ontario who had been in vegetative state for 12 years, into an fMRI scanner and asked if he was in pain. The patient while in the scanner was told to imagine walking around his house if the answer was "yes" or playing tennis if the answer was "no".
"Do any parts of your body hurt right now?", Owen asked.
No, came the answer. Juan Torres, a patient from Toronto, six years after a catastrophic brain injury at age 19, re-enrolled at university.
"He's intellectually right back to where he was before", noted Dr. Owen of the exceptional recovery.
"Twenty years ago, people would say to me, 'isn't there some sort of surgery you could do to fix these patients? Well, maybe, but we didn't know where to start. You need the basic imaging and you need to understand what's causing the problem before you can solve the problem of how to fix people."
"And I think we're getting there. We're just at the tipping point right now." Dr.Adrian Owen
"We've got patients who we know are on the edge of being able to establish communication, but we don't really know what to do for them yet."
"Just because we identify consciousness and awareness, it's not enough. It's terrible to know we can make these measurements, identify awareness and not be doing what needs to be done, which is to build a medical infrastructure to support these people."
Dr.Nicholas Schiff, neuroscientist, Weill Cornell Medicine, New York
In 2007, Dr. Schiff was the lead author of a study published in
Nature describing a 38-year-old man who had been over five years in a minimally conscious state. Now that man is able to communicate with his family. He was the recipient of electric current pulses to his brain, a therapy called deep-brain stimulation
(DBS). Through stimulating the central thalamus whose job it is to relay motor and sensory signals to the cerebral cortex, that part of the brain involved in consciousness, Dr.Schiff's team helped this patient to name objects, to produce hand gestures, and to eat without the use of a feeding tube. Even years after the occurrence of a catastrophic brain injury DBS
"can promote significant late functional recovery from severe traumatic brain injury".
 |
| Juan Torres at his home in Oakville, Ont. (Photograph by Cole Garside) |
Labels: Brain Injury, Medicine, Research, Therapy, Vegetative State


:max_bytes(150000):strip_icc()/marijuana-and-anxiety-1393132_FINAL_2-cceefa528c5c44c698e11eacb72a0a29.png)


























/cdn.vox-cdn.com/uploads/chorus_asset/file/7724917/Artboard_1.jpg)

